What is PWS?
Prader-Willi syndrome is a complex genetic condition. Various studies have shown that between 1 in 15,000 to 25,000 children are born with Prader-Willi syndrome and it affects all races and both sexes equally. Prader-Willi syndrome is rare and most people, including many physicians and caregivers as well as new parents and family members, are not familiar with this syndrome. We have produced a collection of guides and resources about Prader-Willi syndrome for families, medical professionals and other people involved in the care and support of people with Prader-Willi syndrome.
Cause
Prader-Willi syndrome is a genetic condition whose cause is quite complex.
It occurs when there is lack of expression of one or more genes in a specific region on the chromosome 15 that was inherited from the father, the precise location of the abnormality being designated as 15(q11-q13).
There are 3 common ways that this lack of expression can occur:
• there is a missing segment at this location from the chromosome 15 that was inherited from the father, called a deletion (found in about 70%);
• the entire chromosome 15 contributed by the father is missing and instead there are two chromosome 15’s inherited from the mother, which is called maternal uniparental disomy 15, or UPD 15 (found in about 25%), or
• there is a defect in the normal expression of the relevant genes due to an abnormality in control of gene expression, called an imprinting defect (found in 5% or less). The syndrome generally occurs as an isolated event in the family and risk is low that parents with one affected child will have another child with the same condition in the vast majority of families.
There is nothing that either parent did or did not do, either before or during the pregnancy, that causes this genetic alteration.


What are the symptoms of PWS?
Physical characteristics:
There is usually a characteristic facial appearance with a narrow forehead, almond-shaped eyes, and a thin upper lip with downturned mouth. However, where children with Prader-Willi syndrome receive growth hormone this is much less obvious. Scoliosis (S-shaped curvature of the spine) may develop. Many individuals with Prader-Willi syndrome who have the deletion type have fairer colouring of their hair, eyes and skin compared to other family members.
Growth deficiency:
People with Prader-Willi syndrome typically have short stature compared to the family height and small hands and feet. Early growth may be below normal, and there is failure to have a pubertal growth spurt, although treatment with daily growth hormone will correct this problem and height may then be normal.
Hyperphagia (drive to eat):
People with Prader-Willi syndrome have an abnormality in the part of their brain (the hypothalamus) that helps determine changes in feelings of hunger before and after eating. They have this continuous urge to eat that is very different from the period of poor eating in the early years. In addition, they need fewer calories to maintain an appropriate weight. This is believed to be due to decreased muscle tone and bulk and lower physical activity.
It is important to provide the needed nutrients while restricting calories in order to maintain a healthy weight. Access to food must be limited and regular (preferably daily) exercise should begin as early as possible. Weight management should be individualised and may include weekly weighing, complete control of food intake and environmental barriers to food access (such as locks on kitchens).
Incomplete sexual development:
The small genitalia that characterise affected individuals are more easily identified in males, but affect both sexes. Males often have undescended testicles and a small, poorly delineated scrotum; females have small labia minora and clitoris. Pubertal development is typically delayed and incomplete, and fertility is extremely rare and has occurred only in females. Hormone treatment during adolescence may be recommended.
Intellectual disability:
Learning, social and cognitive development is delayed and impaired. Although there is wide variability in abilities most people with Prader-Willi syndrome function below what would be expected given their family background and the average IQ for people Prader-Willi syndrome is around 60, which is in the mild intellectual disability range. People with Prader-Willi syndrome may have other specific impairments affecting their social functioning, working memory, and their ability to change their attention from one task to another.
Speech and language difficulties:
The great majority of people with Prader-Willi syndrome develop spoken language and can communicate verbally. Cognitive capacity and probably also the extent of hypotonia may affect the development of these abilities and speech therapy may be helpful and the use of symbols and visual material may be valuable.
Balance and Coordination:
Fine motor skills (the use of hands and wrists to make precise movements) usually are well developed, while gross motor skills (relating to the use of the torso and limbs for example in running and for balance) remain limited.
High pain threshold and irregularities in body temperature control:
Most people with PWS are unaware of injury and infection because of blunted sensory mechanisms and reduced sense of pain. Unexplained high or low temperatures may occur and there is often insensitivity to environmental temperature. Complaints of pain should be taken seriously as when they occur they may indicate serious illness.
Scratching and picking:
Many individuals with Prader-Willi syndrome pick and scratch at sores and insect bites which, if not controlled, may become chronic sores and result in infection.
Behaviour, mental health and temperament:
Children with Prader-Willi syndrome can be loving and happy particularly in the early years. However temper outbursts and subtle changes, typically mood swings and behaviour difficulties may emerge over time. Some teenagers or adults with Prader-Willi syndrome can develop more serious mental health problems.
Other findings:
People with Prader-Willi syndrome may experience excessive daytime sleepiness and sleep apnoea, particularly if obese. Eye abnormalities such as strabismus (cross-eyed), myopia (near-sightedness) or amblyopia (lazy eye) are common.
Treatment and intervention
There is currently no cure for Prader-Willi syndrome, nor is there a drug that can be prescribed to alleviate all of the symptoms and there is no known treatment to lessen the drive to eat, although much research is being conducted in this area. However, the lives of people with Prader-Willi syndrome can be transformed through having a sound understanding of the syndrome and access to good informed care and support.
Treatment is primarily symptomatic and most importantly consists of:
- Early diagnosis, provision of information and support with interventions.
- Lifetime weight control through diet, environmental controls (limited access to food), and exercise.
- Growth hormone replacement therapy when available.
- Sex hormone replacement therapy when available
- Support strategies that seek to minimise behaviour difficulties and which support activities and social engagement that helps maintain wellbeing
With appropriate support and information and the effective management of specific aspects of the syndrome, people with Prader-Willi syndrome can expect to live healthy and increasingly long lives.
How a child with PWS develops
The pattern of characteristics associated with Prader-Willi syndrome is consistent among those affected by it, although there is significant variability in severity and not all individuals affected have every characteristic.
As a simplification, the syndrome is marked by distinctly different presentations in infancy compared to childhood or later in life.
Initially, a baby will present at birth with very low muscle tone resulting in a floppy baby (hypotonia), slightly low or normal birth weight and a poor suck. Subsequently there may be a failure to gain weight and grow well and delayed developmental milestones.
Both boys’ and girls’ genitals are often poorly developed at birth, and one or both testes are usually undescended in males. Because of the weak, limp muscles and poor suck, infants are almost always unable to nurse and often require special feeding techniques such as special bottles or tube feeding.
The milestones of lifting the head, sitting up, crawling, walking, and speech all tend to be delayed. On average, independent sitting is achieved at around 12 to 13 months, walking at 24 to 30 months, and tricycle riding at 4 years. The first word may appear around 21 months and sentences around 3.5 years. The early use of growth hormone and intervention from disciplines such as physiotherapy and dietetics is important at this early stage.
Early in life there follows a period of what appears to be normal eating behaviour and improvement in muscle tone and in physical activity. However, this in turn is followed by a phase that is usually marked by an increased appetite and often a compulsion to eat. This often occurs in toddlers or young children.
With the onset of this stage life becomes dominated by the child’s excessive appetite and drive for food. Individuals with Prader-Willi syndrome do not feel full after eating (lack a sense of satiety) what for others would be a normal or even excessive amount of food. If they have free access to food children and adults with Prader-Willi syndrome are known to eat large amount of food without becoming nauseated or having indigestion and many have never vomited.
This striving for food combined with a lower than normal calorie requirement, and often the decreased physical activity related to the hypotonia, results in rapid weight gain. If access to food is not supervised, severe obesity is very likely to occur and leading eventually to the consequences of obesity including: respiratory difficulties, heart disease, diabetes mellitus, severe swelling of the ankles and feet, sleep abnormalities and other problems. These health problems can be prevented with appropriate control of the food environment.
What is the treatment for PWS?
There is currently no cure for Prader-Willi syndrome, nor is there a drug that can be prescribed to alleviate all of the symptoms. As of this writing, there is no known substance that has been demonstrated to lessen the drive to eat, although much research is being conducted to find such a substance.
Treatment is primarily symptomatic and most importantly consists of:
-
Early diagnosis and intervention
-
Lifetime weight control through diet, environmental controls (lack of access to food), and exercise
-
Growth hormone replacement therapy, when available
-
Behaviour management , with consistent limit-setting
-
Special education and sheltered or supported employment
Early Diagnosis
Early diagnosis of PWS gives parents an opportunity to manage their child‘s diet, prevent or treat infantile failure to thrive, avoid obesity from the start, and improve behaviour. It may facilitate a family‘s access to critical early intervention services and help identify areas of need or risk. It allows families to know what to expect and institute appropriate preventative measures.
Weight Control
People with PWS have a flaw in the part of their brain that determines hunger and satiety that gives them a continuous urge to eat following their period of poor eating in the early years. In addition, they need fewer calories to maintain an appropriate weight. This is believed to be due to decreased muscle tone and bulk and lower physical activity. It is important to provide the needed nutrients while restricting calories in order to maintain a healthy weight. Access to food must be limited and regular (preferably daily) exercise should begin as early as possible. Weight management should be individualised and include weekly weighing, complete control of food intake, environmental barriers to food access (such as locks on kitchens) and diets acknowledging that fewer calories are required.
Growth Hormone
In recent years, numerous studies have demonstrated conclusively that growth hormone replacement therapy can very positively affect growth, body composition (the proportion of fat to muscle and bone), and activity level in people with PWS. It can also improve breathing and probably also speech and academic performance. Since it can improve body shape and physical abilities, it also improves self-image. However, growth hormone requires a daily subcutaneous injection, is expensive, and is not covered by all health programs in all countries..
Behaviour Management
Behaviour management is crucial for both weight and behaviour problems. Behaviour management should be oriented towards intervention and prevention. Consistent enforcement of limits by all caregivers (including parents, the wider family, teachers, and residential carers) is very important. For the best results, make a schedule, plan the day, avoid arguments and anticipate what issues may arise.
Special Education and Sheltered or supported Employment
Because of the developmental delay and intellectual disability combined with the behavioural problems, people with PWS require special assistance in school in order to learn as much as their abilities allow. Once they have completed school, they need assistance in finding employment that matches their abilities optimally, and supervision to control access to extra food and deal with behavioural outbursts when they occur. Adults with PWS who do not live with their family will require a residence that includes supportive supervision and accommodation to their dietary and behaviour control issues while simultaneously allowing them as much success and social interaction as possible.
What are the clinical features of PWS?
The pattern of characteristics associated with PWS is consistent among those affected by it, although there is significant variability in severity and not all affected individuals have every characteristic.
As a simplification, the disorder is marked by distinctly different presentation in infancy versus later in life.
Early phase
Initially, the neonate presents with slightly low or normal birth weight and poor suck with subsequent failure to gain weight and grow well, very limp muscles, and delayed developmental milestones. Genitals are often small in both sexes, and one or both testes are undescended in males. Because of the weak, limp muscles and poor suck, infants are almost always unable to nurse and often require special feeding techniques such as special bottles or tube feeding (gavage). The milestones of lifting the head, sitting up, crawling, walking, and speech all tend to be delayed. On average, independent sitting is achieved at around 12-13 months, walking at 24-30 months, and tricycle riding at 4 years. The first word may appear around 21 months and sentences around 3-1/2 years.
Second phase
There follows a period of normal eating behavior and improvement in muscle tone and activity. However, this in turn is followed by a phase that is usually marked by an increased appetite and often a compulsion to eat. This often occurs in toddlers or young children. Life becomes dominated by a voracious appetite and drive for food. Individuals with Prader-Willi syndrome apparently do not feel full (lack a sense of satiety). They can eat a tremendous amount of food without becoming nauseated or having indigestion – and many have never vomited. This striving for food combined with a lower than normal calorie requirement and, frequently decreased activity related to the hypotonia will result in rapid weight gain if not controlled externally, leading to obesity and eventually the consequences of obesity: respiratory difficulties, heart disease, diabetes, and other problems.
Diagnosis
Prader-Willi syndrome is usually suspected on the basis of the clinical signs and symptoms (see above) and confirmed by genetic testing. Clinical diagnostic criteria have been published in the medical literature and confirmed as accurate. However, because other disorders can have overlapping manifestations, the diagnosis should be confirmed by genetic testing, which is clinically available in many countries and is very accurate. Currently, the best test for Prader-Willi syndrome is called methylation analysis, and it is the best because it will be positive regardless of the genetic type. Other genetic tests can be used to determine the specific type, if that is desired, but it is not necessary to confirm the diagnosis.
If testing is not available in your country then you may be able to access free testing by using our service based in Italy, or if you are based in South America then another service is available.
More information about PWS is available on request. Please enter your name and email address below.
International Community
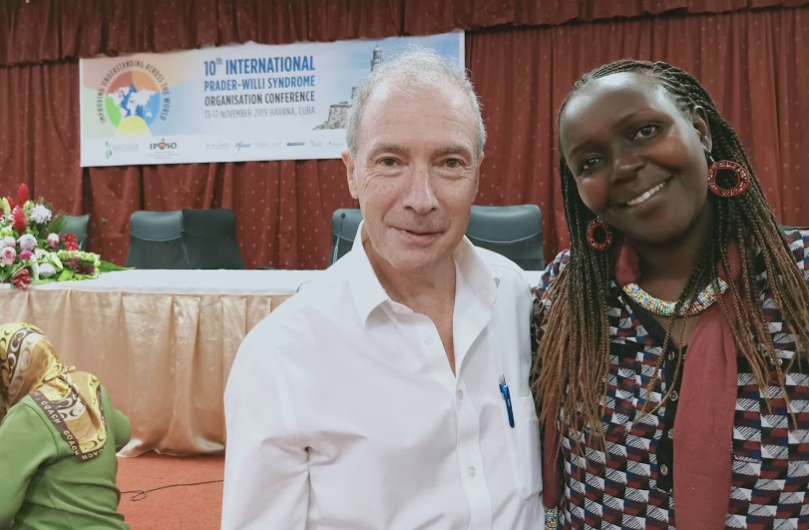
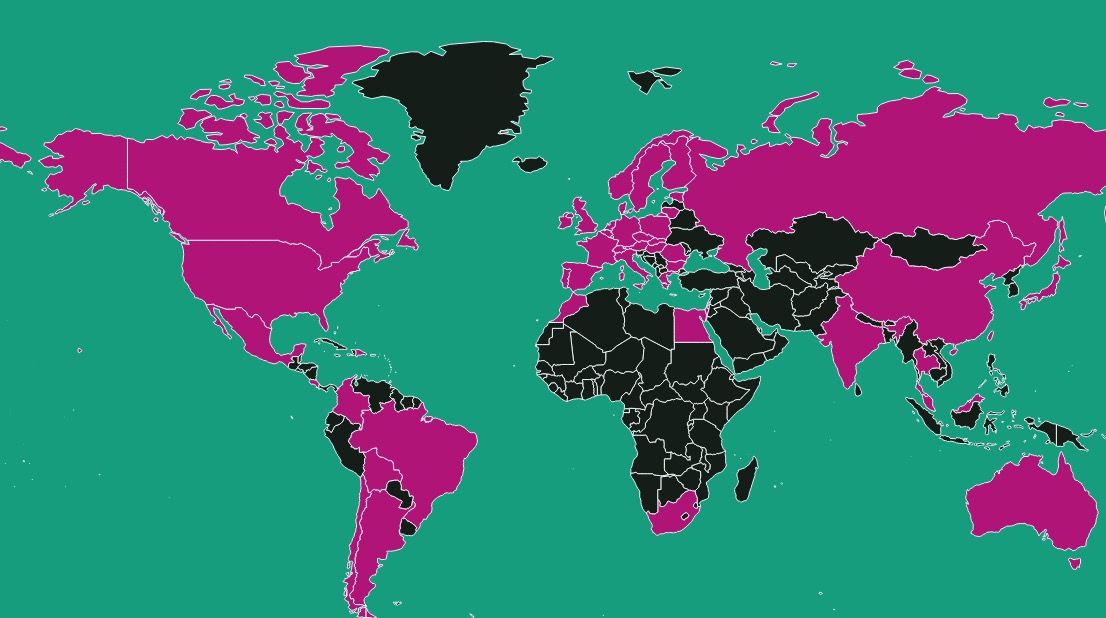
IPWSO was established so that PWS associations, families, clinicians and caregivers around the world could exchange information and support and have a united global voice under one umbrella.
Information for Medical Professionals
The latest medical and scientific research and information, plus guides into common medical issues affecting people with PWS.
What is PWS?

Prader-Willi syndrome is a complex genetic condition. Various studies have shown that between 1 in 15,000 to 25,000 children are born with Prader-Willi syndrome and it affects all races and both sexes equally.
Free Genetic Screening

If you suspect your patient has Prader-Willi syndrome, based on the clinical signs and symptoms, but are unable to access testing in your country, then you may be able to access free genetic screening.